Proposed Changes in The Medicare Physician Fee Schedule Will Challenge Your Compensation Plans
CMS announced proposed policy changes for Medicare payments under the Physician Fee Schedule (PFS) and indicated that it will waive the 60-day publication requirement for the Final Rule and replace it with a 30-day notification. This means that the Final Rule will be effective January 1, 2021 even though it may not be published until December 1st. If implemented, one of the most significant provisions includes material changes in the Resource-Based Relative Value System (RBRVS).
The RBRVS changes are proposed to achieve two primary goals:
- Through increased reimbursement, recognize changes in medical practice and the relative value of services for “cognitive” specialties (e.g., primary care, neurology, nephrology, etc.); and
- Be budget neutral which, under a model rewarding “cognitive” specialists, requires a reduction in reimbursement to “procedural” specialties (e.g., surgery, gastroenterology, etc.).
These goals will be accomplished primarily through two changes:
- Changes to the Work RVUs (WRVUs) assigned to individual CPT codes – most notably, increased WRVUs assigned to the E&M CPT codes which represent the largest source of revenue for cognitive specialties. Two new E&M codes are also proposed to be added; and
- Reduction in the conversion factor (which determines payment levels) by 10.6 percent.
The net impact to Medicare expenditures will be budget neutral. However, individual physicians will observe wide swings in WRVUs and Medicare reimbursement. Reimbursement from commercial payers could also be impacted if those contracts are tied to Medicare rates.
Impact on WRVUs and Physician Compensation
While the RBRVS system was developed as a mechanism to determine Medicare reimbursement levels, WRVUs have become a universally accepted metric to measure physician productivity and work effort and serve as the basis to determine physician compensation and incentives in the majority of physician compensation models. Thus, while CMS’s intent was to address reimbursement disparity, the changes result in potentially unintended consequences on compensation plans that are based on WRVUs.
Table 1 illustrates the estimated impact on WRVUs on selected specialists, whereby the largest increases are expected in the more office-based specialties.
Table 1
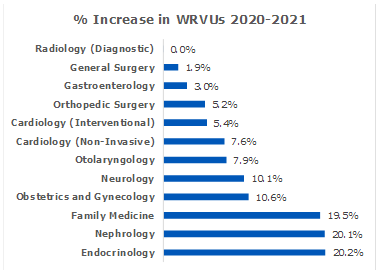
1 Source: Veralon analysis based on 2021 PFS proposed by CMS and the procedure frequency distribution by specialty as reported by Medical Group Management Association.
WRVUs for most physicians will increase at least somewhat. But reimbursement will only be redistributed, and the impact will vary based on your mix of physicians.
The impact of these changes may be summarized as follows:
- Physicians whose WRVU totals are increasing significantly (due to a high volume of E&M procedures) will, without mitigation, earn higher compensation levels if paid based on WRVU productivity. While the economic impact on practices for physicians with increased WRVUs may be mitigated by a redistribution in Medicare (and potentially some commercial) reimbursement, we expect a net negative financial impact;
- Physicians whose WRVUs increase more modestly (because E&M procedures represent a smaller portion of the WRVU total) will, without intervention, earn modest compensation increases. However, health systems will observe a negative net economic impact caused by reduced reimbursement to these specialists.
We believe health systems need to take proactive steps to understand and potentially mitigate the negative financial impact caused by these compensation changes.
What Can You Do?
This will be an iterative process whereby organizations may need to ultimately make material changes to their compensation plans. In the meantime, we suggest several actions for consideration.
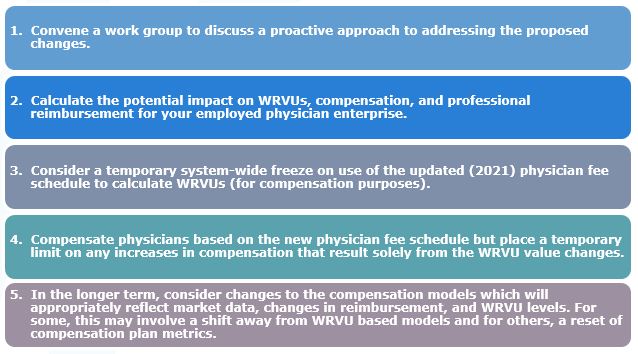
Doing nothing leaves the organization vulnerable to significant financial consequences, and potential compliance risks.